The hospital staffers who watch heart rhythms are usually “telemetry” technicians, not nurses. At HCA Healthcare facilities, they may monitor as many as 80 patients at a time.
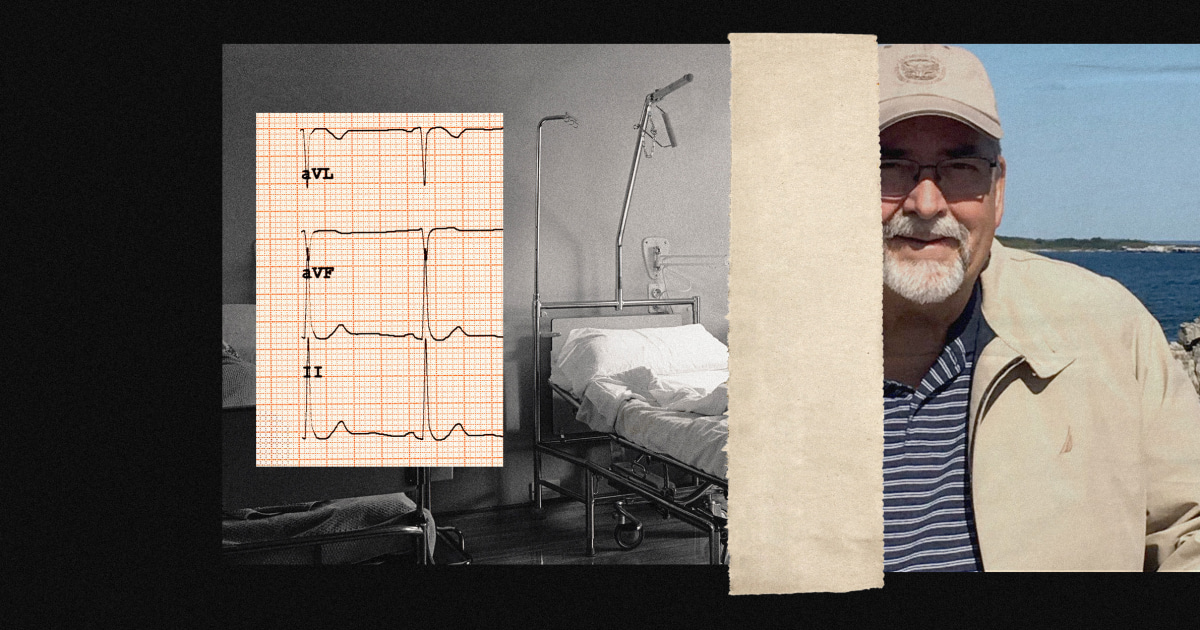
After three harrowing weeks in the hospital, Terry Downs, 68, was on a path to recovery. A former Boeing engineer who helped design the stealth bomber, Downs was admitted to HCA Healthcare’s Wesley Medical Center in Wichita, Kansas, in July 2022 with what was found to be a brain bleed. By month’s end, he was scheduled for discharge from the 760-bed facility and headed for rehabilitation.
He never made it. In the wee hours of Aug. 1, a nurse walking by his room heard him choking and found his heart barely beating. A half hour earlier, his pulse had been strong, Downs’ 2,200-page hospital record shows, but when his heart rhythm changed, no one assigned to monitor it had alerted nurses.
In Wesley Medical Center, and in most hospitals today, the people monitoring patients’ heart rhythms, blood pressure or respiratory functions are not nurses who interact with them. They are “telemetry” technicians who are supposed to alert those nurses to meaningful changes in the vital signs transmitted by electronic devices hooked up to the patients.


Seems from the article that it’s about the telemetry techs being overworked:
…
…
This seems like bad design. Not that it’s monitored remotely but that it needs a person as the only monitor. We should be able to get the frequency of the heart beat and the amplitude, not as a picture but as numbers. Once in number form it should be easy to program a system where say (making up numbers as I am not a doctor) a change of > 5% in frequency or a change of <10 % in amplitude triggers an automatic signal to the nurse.
A person should not decide “is that significant enough to trigger a call”
Talking about bad designs, check this out:
The system should monitor it, and pop up a alarm when something is unusual, with say the last 5 minutes of data, and then the person monitoring should relay all pertinent info to a nurse.
Although at that point why not send the information directly to the nurse?
The problem is you’re asking hospitals to spend a few million in licensing fees for such a system. That shit has to be FDA approved, which is extremely expensive.
That’s harder to get approved because the finance people only think a quarter at a time.
Remember, if there’s a bug in your code, people will literally die.
I work in medical devices and understand the cost/responsibilities of of Healthcare systems.
That said we don’t need any new monitors. We can detect a person’s heartbeat. To display it on the screen we must have the frequency and amplitude. As I said I’m not a doctor so I can’t say what should be a “alarm” situation but we must know this since we teach people to do it.
The biggest issue is converting human talk to machine code which is not a large barrier. The financial gains are huge, these “telememetry nurses” can’t be cheap. A company makes this for say 20 million(no new technology, regulatory submission and some programmers). Sell it to hospitals for 20k a year…
How many hospitals would turn down reducing headcount by 30-70 people at 80k each(not net but including insurance and pto and holidays etc etc, just estimating) for a single bill of 20k a year? Hell go 10x and charge 200k, still an easy sell.
This is the perfect application of the new ML we have available.
The idea seems obvious but if have the backing to get through regulatory submissions hit me up.